|
| Clinical Picture and movements at presentation |
This 15 year old girl was a precious child for her parents, born after many attempts of IVF.
She had a short and bowed forearm, and in addition had an unsightly prominence in the lateral aspect of the elbow.
She also complained of pain when she had to do any writing tasks for a long time.
 |
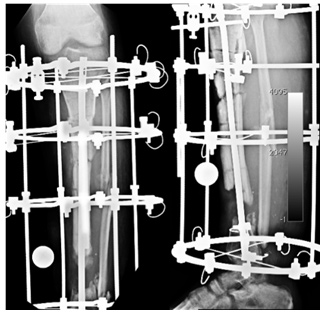
| Xray at presentation |
Xrays revealed an exostosis at the distal ulna, which caused a short ulna, which in turn by the check rein effect caused an exaggerated bowing of the radius and dislocation of the head of the radius. Some surgical procedure had been attempted in the past, details of which were unavailable.
The challenge here was to correct the bowing deformity, as well as the prominence of the radial head, without much surgical scars.
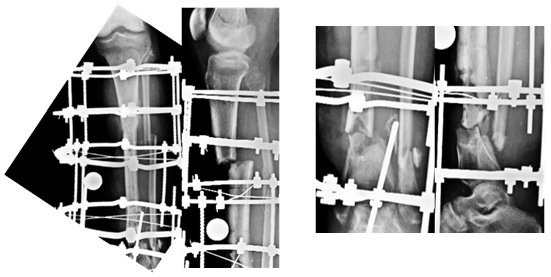
We first excised the ulnar exostosis. 6 weeks after that, we applied a pediatric LRS fixator on the ulna.
The trick here was to put in the proximal and distal set of pins without the rail, such that each set of pins was perpendicular to that segment of bone.
 |
| C arm pictures of fixator application & osteotomy |
Once the clamps were fixed to the rails, the bowing of the ulna was automatically corrected.
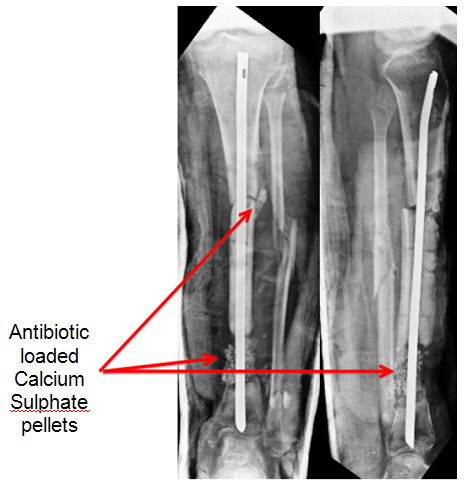
Due to the acute correction, instead of the normal 7 days, we began lengthening after 10 days, and continued lengthening, till the distal end of the ulna reached the carpus / distal end of radius.
 |
| Sequential Xrays of Ulnar Lengthening |
 |
| C arm pictures of insertion of Screw and K wire |
 |
| The Radial Head moves distally |
 |
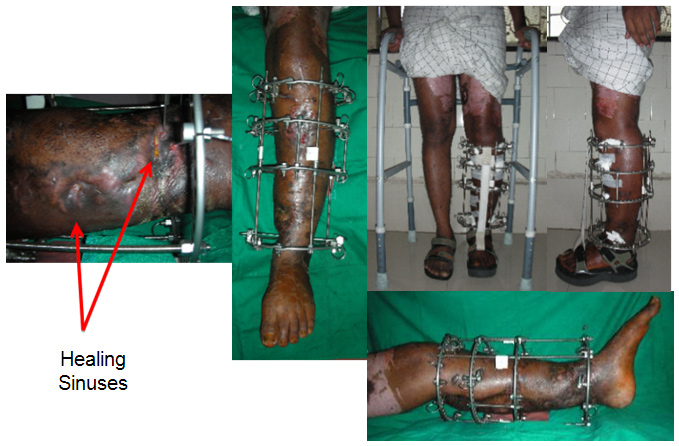
| Function with the Fixator |
 |
| Healed regenerate |
 | |
| Scars and Prono-Supination |
At her one year followup, she is obviously a happy patient, free of her deformity, and her complaints.
Notice the the bump of the radial head is hardly (if at all) visible.
She is now back at her village, attending Junior College.